The Shirley Ann Jackson, Ph.D. Center for Biotechnology and Interdisciplinary Studies (CBIS) at Rensselaer Polytechnic Institute is a powerhouse of fundamental and translational research tackling the most pressing health care and biotechnology challenges facing humanity.
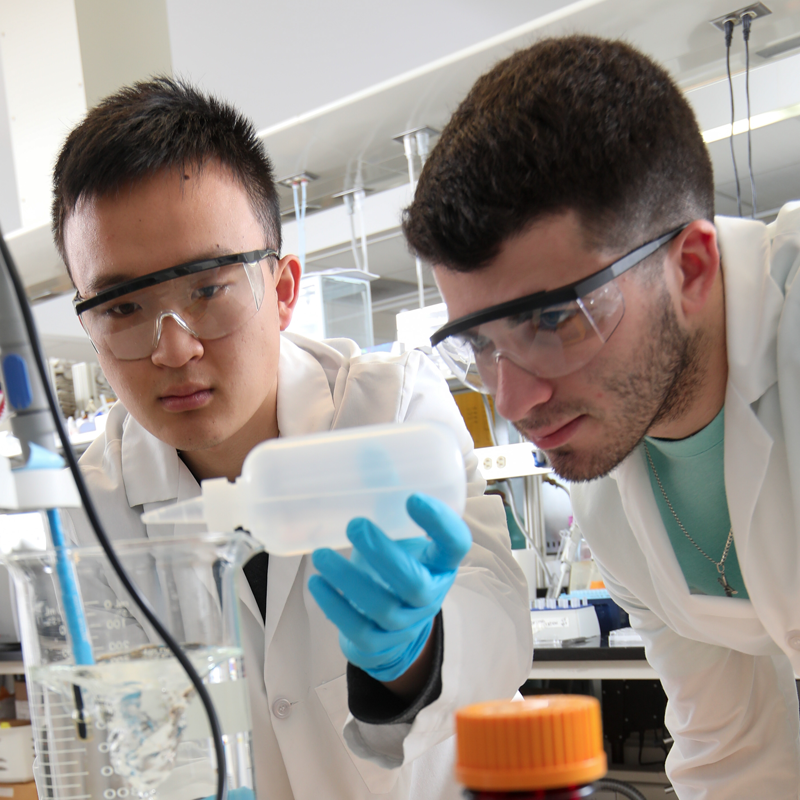

36
Resident Faculty
148
Graduate Students
11
Core Facilities
$18.7
Million in Research Expenditures

